I presume that I am asked to talk on this subject because there are now so few of us left who can talk about it at first hand. I have always been interested in history, and now, to my surprise, I find myself part of it. I retired 25 years ago at the age of 60, and (to save you getting out your slide rules) this makes me 85 this year. This evening I intend to spend more time on the first 30 years and less on the last 30, which will be much better known to you.
First, something about myself. I took my London B.Sc. in June 1941 having already decided on a career in Medical Physics. Soon after, I went to see Prof. Mayneord at what was then the Royal Cancer Hospital (Free). This was long before the NHS when most hospitals were charities and had to raise as donations the money required to run them. Some chose a title which they thought might help in this. After the NHS came in, the Royal Cancer Hospital (Free) became the Royal Marsden Hospital. Mayneord had nothing to offer me, but commented that in those days a hospital physicist was worth his weight in radium. He referred me to Prof. Russ at the Middlesex Hospital who was running a scheme to enable a physicist to be available to any hospital in London needing a physicist but without one because of the War, and the physicist then in post was one Frank Farmer. As from December he would become a lecturer in the Medical School, so I was appointed to understudy him and take over from him.
In those days the work of a hospital physicist was almost entirely concerned with the treatment of cancer, involving the calibration of X-ray therapy machines and also the use of radium which was restricted in London because of the danger of bombing. Generally, radium was then stored in a bore-hole like that at the Middlesex, but we could store small quantities locally in a specially made type of steel container. This was about 1 ft in diameter, and some 15 inches high with a 2" diameter hole in the centre sealed by a steel plunger which had a screw thread more than 2" in length. A brass container fitted into the bottom of this hole long enough to hold the longest radium needles in use, 10 cm. One of these steel containers had been tested at Woolwich Arsenal alongside a bomb and it just bounced beautifully.
It was permissible to use radium clinically only if the patient could be nursed in a reasonably safe area, which at UCH was the sub-basement of the Private Patients' Wing. A bomb actually exploded in the radium room of one London hospital and the whole building immediately collapsed on top of it. A long search found one of the two radium containers in the rubble. Weeks later it was found that the bomb must have exploded close to the second container, blowing it across the courtyard and into the opposite wing which then collapsed on it. However, all the radium tubes were undamaged and ready for clinical use, thanks to the strength of these containers.
Radium had been widely used before the War, mainly for interstitial and intra-cavity treatments. To reduce the hazards from bombing, some 4 gm of radium (i.e., about 150 GBq as RaBr in HBr solution) was lodged in a tunnel (part of an old lime-kiln) in the Chiltern Downs near Luton. This was in a plant from which the first daughter product of radium, the gas radon, could be extracted daily and sent to hospitals all over the country. The gamma radiation emitted was exactly the same as if radium were used, but the half-life was about 4 days instead of some 1600 years. So until December I spent some time each week at the Radon centre and the rest at the Middlesex understudying Frank Farmer.
Prof. Russ had been one of the founder members of the British X-ray and Radium Protection Committee in 1921 whose recommendations were the first in the world on the subject. But even by 1941 radiation protection was still of minor concern compared with today; there were certainly no regulations or Codes of Practice, and few recommendations. In diagnostic radiology it was accepted that any patient would only get X-rayed very occasionally and then only receive such a small dose of radiation that any effect would have worn off before the next examination. I was asked to measure the radiation received by some such patients, and quickly found that surprisingly high doses could be received, for example, by barium meal patients. A number of these received doses to parts of the back of tens of rad, the highest being about 300. This was largely due to fluoroscopy then being carried out without any intensification of the image. I also found that in one particular projection of a patient in late pregnancy the dose to the gonads of the f›tus could also reach tens of rad. I was at that time one of three people in Britain who were making such measurements, and our work began to cause concern over the amounts of radiation that could be received by diagnostic X-ray patients.
During my time at the Middlesex when I was working with Frank Farmer, he was beginning his work on electronic instruments for measuring ionising radiation, long before transistors were available. His first contained an electrometer valve having a long stem of very high insulation glass, with the grid connection at its end. Up to this time, the conventional method of measuring the strength of a radioactive source (e.g., a needle containing radium) involved using a gold leaf electroscope. Does this instrument still feature in the B. Sc. curriculum, or is it now relegated to A-level, or even O-level, work? I found that the work was easier on the eye, and the results less variable, if the gold leaf was only used as a hinge for a graphited thread.
During this time the idea was mooted that it might be possible to build an electronic metal detector to assist a surgeon in the removal of metallic foreign bodies. This was long before the days of metal locators, and in the early days of superhet radio receivers. Everyone knew that movement near the coils of the tuned circuit of a radio receiver could alter the frequency of that circuit and cause the old familiar howls. Together with Frank I played about with this for a bit, and we decided that it was not likely to be very useful, but we published a brief note in the Lancet about it.
In 1942 I saw an article in the Reader's Digest by an American surgeon which said how useful such a device had been in their hospitals after the Pearl Harbor attack. I wrote to him asking about his instrument, and in his reply he had no intention of letting me know how it worked. A year or so later I had a further letter from him offering a metal detector free; if we wanted it, he would get it sent over next time an American bomber was coming across the Atlantic with supplies for war-torn Britain. It duly arrived, but by this time Frank had moved to Newcastle, and I had moved to UCH, so we reckoned that we owned the machine jointly. It would be lodged with one of us, and if the other needed it it would be sent on the next mainline LNER express, to be collected from the guard personally. It was good at detecting iron and steel, very poor for non-magnetic metals, and useless for anything else.
I had already seen operations for metallic foreign bodies last for hours, with the metal not found at the end. With this machine such operations were very much faster, and almost always satisfactorily. Indeed, the fastest such operation I witnessed took 17½ seconds by the theatre clock from skin incision to removal.
The American machine, the Berman Locator, used a ferrite core for the tuned coil just below the tip of a sterilisable plastic sheath. A later model used a higher frequency, and this enabled non-ferrous metals to be detected though with reduced sensitivity. I was interested to see recently that commercial metal detectors are now being used instead of X-rays just to determine the presence of metallic foreign bodies. The Berman instrument was a locator, not merely a detector, and designed to be used in the theatre. There was one at UCH when I left in 1962, and I see that it still exists - in the museum cupboard.
In 1941 London, the blitz was coming to an end, but still with air-raids almost every night, and often by day as well. The big London teaching hospitals were mostly evacuated to places in the Home Counties where a stately home, or an underused mental hospital, had grounds sufficiently large for the required wards and laboratories to be built as prefabricated structures.
I visited one during my time at the Middlesex to calibrate the output of a superficial X-ray therapy machine being used by a dermatologist for treating skin cancers. In the early days of radiotherapy three units of dose had been used - Threshold Erythema Dose (TED), Pastille dose (B dose) and Röntgen dose (r dose), although by the 1940's the first two had been almost totally superseded. The dermatologist asked if I had brought my pastilles, and I replied "NO", but instead I had brought a Victoreen r-meter which measured doses in röntgen units. He said that he didn't mind so long as I told the radiographer how many pastille doses there were to one r unit. I replied that, for the radiation he was using, there were about 300 r units to one pastille dose. (For radium gamma - rays, the figure would be nearer 10,000). When I had finished, I was packing up when the radiographer asked for help. Before leaving, the dermatologist had told her to select a medical student and treat a 1 cm diameter area of his upper arm with a dose of what I said was 1¼ pastille doses. He would be in the next day and see from the skin reddening whether I had done my calibration properly.
A visit to another such hospital was to search for two small radium needles. For inserting radium into tissues, it would be packed tightly into a platinum tube of about 2 mm diameter and up to 10 cm long, sealed with gold solder. For superficial or intra-cavitary application, it would be packed into similar tubes, but much shorter and some 5 mm in diameter. This patient had a cancer of the lip, and three small needles had been inserted some days previously. He was of low intelligence, found the needles irritating, and had pulled two of the three out. When this was discovered, the staff searched the ward without success, and then called for help. I got there to see a sight I never expect to see again. The Medical Superintendent, the Hospital Administrator, and the Hospital Matron were together searching the patient's bed trying yet again to find the missing needles. We had no Geiger counters in those days, and the search instrument was known as the "clucking hen" [Ref 1]. This instrument told me that there was radiation present, which turned out to be from the third needle still in the patient, sitting quietly beside his bed. He was moved away, and no further radiation was detected. I asked where the floor sweepings would go - into the incinerator. This turned out to be a gently smoking corrugated iron structure half buried in the ground at the furthest corner of the estate. I confirmed that gamma radiation was coming from this, and asked for the contents to be raked out. Old Bill had been a gardener on the estate before the war, so he came to help after wisely filling his pipe with something that gave off a very, very strong smell. After about half an hour I stopped him while I examined one bundle of material raked out, and found one of the two missing needles. When he said he had cleared everything out, there was still radiation from an area in the middle of the "incinerator". The last needle was found buried in the earth floor under an up-turned half-saucer. Fortunately it was a slow burning and low temperature incinerator, and both needles were still intact and ready for further use. Theo Tulley told me that in similar circumstances he had used an ionisation chamber, but for the required sensitivity it had to be large. He used a standard metal dustbin.
It was one hot Friday afternoon at about 4 pm in the middle of August 1942. The Professor was on holiday in the Lake District, and I, with all of 9 months experience behind me, was the senior member of staff actually in the Department. One of the others, Clifford Walker (later of Exeter) was carrying out a research project for the Professor on people who used luminous paint containing radium for luminising dials of clocks, etc. It had been standard practice for them to fill the brush with paint, and then gently wipe it on the tongue to get a sharp point. Clifford had been all week at a large Victorian house in Hampstead which was used as for luminising, taking breath samples from all the folk working there. The results were quite crazy, and contained far more radioactivity than he expected. It turned out that on the previous Monday the Director had taken delivery of some 50 mg of radium (2 GBq) as bromide in HBr solution in a glass tube in a lead pot, and had put it on his personal research desk. He was then called to the phone, and then took a customer out for lunch, and so on and it was after 5 when he turned round and said "Where was I when all that happened? Ah, radium." But it was NOT on his bench. A search revealed the lead pot, empty. Now this was in the middle of a heat wave, and in due course he found out that the lab boy had had a fit of unaccustomed tidiness. He had taken the tube out of the lead pot, smelled it, and decided that it was just water, so he opened the window and poured it on the wilting flowers in the garden outside. On Wednesday there was a thunder storm. And this was Friday afternoon. I went with Clifford to the premises, and was very worried about the ground where the radium had been poured since in wartime any vacant land was supposed to be used for growing vegetables. So we dug out as much of the soil as we could from there, and loaded it into a garage nearby, not finishing until almost midnight to periodic shouts of "Put that light out". We wired the Professor, who said we should call in the NPL who in those days were the forerunner of the NRPB. They came and got all the soil put into the lower Thames. A few days later, I went there to see if all was now well, to be approached by one of the staff who took me into a magnificent drawing room. She said that this was the room in which she did her luminising, and she kept the paint on a shelf behind her desk, but they also used it in the evenings as a sort of common room for the folk who lived on the premises - was this all right? I said NO.
One day I was looking through some old papers, and I came across a story from 1925. A nominal 50 mg radium tube (i,e, 2 GBq) was found to contain much less than that. It was sent for remaking, when it was found that only about half the nominal content was still there. The National Radium Commission was set up after World War I to collect together all the luminous dials used in the now superfluous armaments, remove the radium and pack it into suitable platinum tubes and needles for clinical use in hospitals throughout the UK. It was packed as the soluble RaBr simply to facilitate handling. However, the seal of this particular tube was totally inadequate, and there was fluid inside. It appeared that the body fluids of innumerable patients had seeped in and dissolved out some of the radium. (The permissible body burden was then 4 kBq.) It was impossible by then to trace those patients, but all the radium in all the country's hospitals was promptly recalled and repacked as insoluble RaSo4 to prevent that ever happening again.
In 1943, Prof. Russ called a meeting of physicists in hospitals and medical schools to discuss setting up an association of hospital physicists - the HPA. There were about 60 of us in the country at the time, and initially we were an informal society of people interested in the subject. Its concern for professional matters did not start seriously until the NHS was being set up in 1945-8.
In those days few of the measuring instruments needed could be purchased, and many had to be made in-house. When I moved to UCH in 1943 I was the Physics Department for my first three years, with a Victoreen r-meter, a lathe, a soldering iron and a typewriter. Every time radium was used in the operating theatre, I was required to be there with my charts, tables and slide rule. After the size and position of the growth had been determined, I would be given about 5 minutes to calculate the number and strength of needles required, their distribution and the length of treatment time required to give the prescribed dose as uniformly as possible to the target volume. In viewing the X-ray films afterwards I usually found that there had been three ideas about the distribution of the needles - one was mine after calculations were finished, the second was that of the surgeon after he had inserted them, and the third was what the X-rays showed. There was sometimes little similarity between the three.
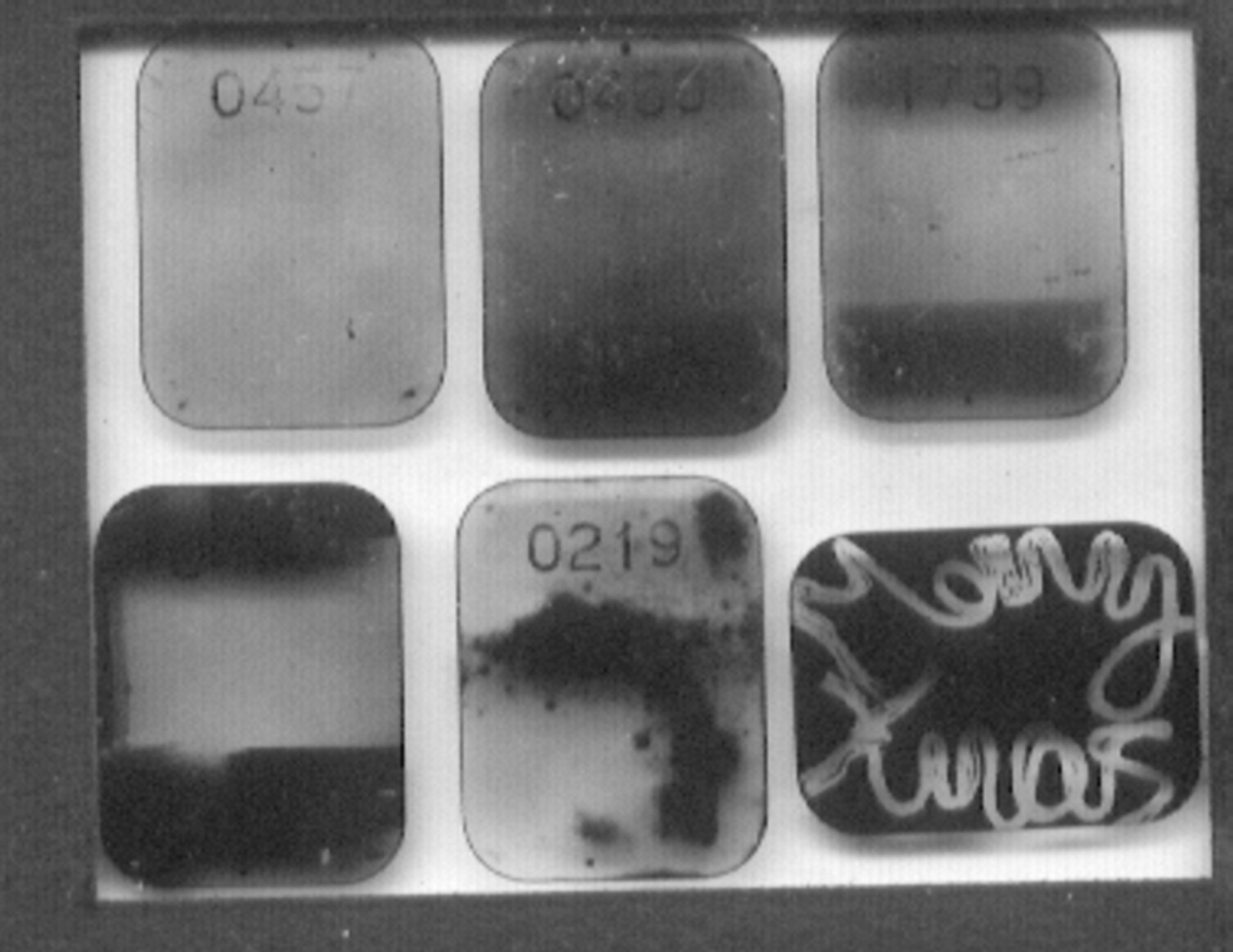
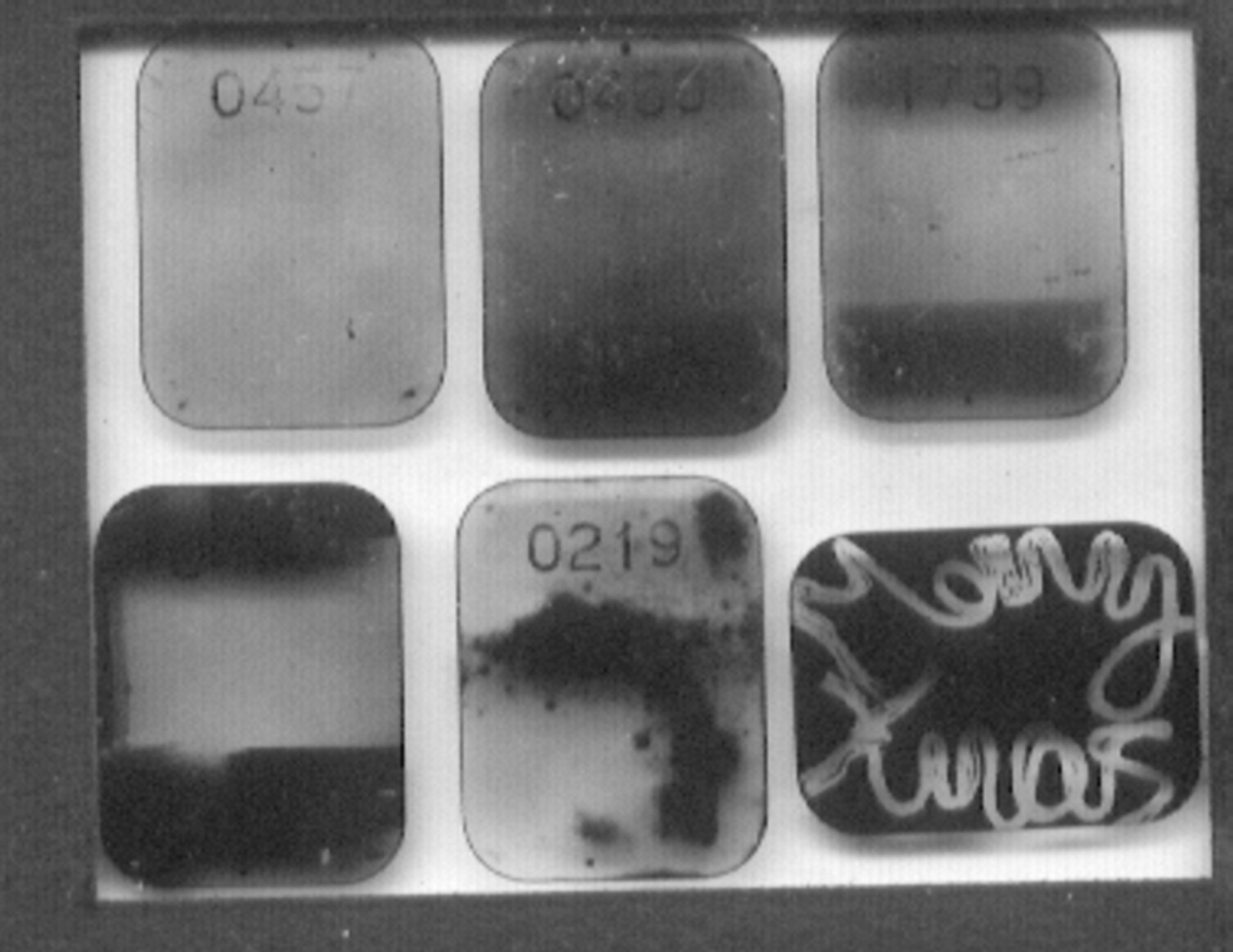
In about 1944 I was asked to measure the radiation received by the staff in the X-ray Department. There were no personnel monitors available, so I adapted a dental X-ray film by partially covering it with thin lead. When I took the first week's results to the Director, he looked down them and called for Dr X . "Ah, Dr X, I have the results of last week's radiation measurements. You only got so much - you're slacking, man!" Unfortunately, these films offered an easy target for jokers [see figure below].
While I was at UCH I was required to join the fire bomb squad to find any incendiary articles that might have landed on the roof, and move them down to the road or wherever before any fire could take hold. This meant being on duty every sixth night. The hospital then existed on five sites, with roads between them, and there were 15 of us on duty at any one time. Three per site. But we could choose where we slept. This was either on the balcony of an empty ward on the 4th floor under a glass roof, or in the sub-basement underneath the hospital's main water intake. Fortunately bombs were never dropped on the hospital while I was on duty.
Immediately after the War there was a General Election at which, to everyone's surprise, Winston Churchill was defeated and Clement Attlee took over as Prime Minister - and one of his election promises was a National Health Service. He chose as his Minister of Health one Aneurin Bevan, a very strong-willed character and this led to a lot of apprehension. In the following three years of intense lobbying and negotiation arrangements were reached that seemed to promise well for the future, especially for the medical profession, and even more especially for hospital specialists. Up to then, as a general rule, in the voluntary hospitals at any rate i.e., those not run by a local authority or other public body, consultants were honorary and unpaid for their hospital duties. The hospital helped them to earn their living by letting them treat private patients in the Private Patients' Wing and charging them fees. In the following years salary structures and scales were drawn up and agreed separately for the many groups of Health Service workers, and the Whitley machinery set up. Before then, each hospital, or group of hospitals, usually fixed salaries quite arbitrarily. I started in 1941 at £200 pa but by the end of the war I had progressed to £550 pa. - riches indeed. We were able to get married and buy our first house (for £1,150 !). I heard from a finance officer at one of London's richer hospitals that they spent 1/3 of all their income on advertising for further donations. Any Hospital Finance Office was therefore primarily a money-raising outfit. Even UCH had a board at one corner of its site appealing for donations to reduce the hospital's bank overdraft of (I think) £500,000.
UCH still had a pre-war unit for external gamma-ray therapy containing about 6 gm. (i.e., about 200 GBq) of radium called a radium bomb because of its shape. The treatment head was built with sufficient shielding of natural uranium for the patient under treatment, as at all other times the radium was kept in a safe linked to the head by flexible tubing. The bobbin containing the radium was moved pneumatically from safe to head for treatment, and then similarly back to the safe after treatment. The tubing was disconnected from the safe every night, and the safe locked. One Monday morning the tubing was wrongly connected, a ring on the end of the flexible tubing being left cross-threaded on the fitting in the safe. As soon as the fan started, the air pressure built up and blew the tubing off the safe, allowing the bobbin to describe a graceful parabola to finish under the sink in the corner of the room. After carefully planning what to do, it was put back into the safe, and the tubing connected properly this time.
Soon after the setting up of the NHS in 1948, the Ministry of Health took ownership of all radium in hospitals and sold it to the Ministry of Supply, who charged hospitals a rental for the use of whatever radium they had. This was not too onerous for small radium needles, but was an enormous charge for the 6 gm in our so-called radium bomb. I found out that we could replace this radium by Co60, and replace this again every three years, for a substantially smaller sum, so we got the required Co60 and told the Ministry of Supply that we no longer needed their radium. This was not well received in Whitehall.
It was probably in the late 1950's when I had a phone call from a somewhat bewildered civil servant who had been given the task of compiling a suitable answer to a parliamentary question asked by an MP. Essentially, the questioner asked how it was that if the new, dirty, thermonuclear cobalt bombs was so destructive, they were being used in some UK hospitals for the treatment of cancer. I pointed out that "cobalt bomb" was the familiar name given to radiotherapy treatment heads incorporating cobalt-60, and had nothing to do with the thermonuclear device incorporating a casing of cobalt. I should have been chuffed to have seen that MP's face when my answer was read.
At the end of the War, we heard about the atomic bombs used on Japan, and took steps to find out what we could about them. Not long after, we heard that the wartime airfield at Harwell was being used for experimental work on nuclear energy under Sir John Cockroft. He soon announced that work was under way to get GLEEP going (Graphite Low Energy Experimental Pile) so that, among other things, small quantities of radioisotopes for research projects, and for medical purposes would be available. He let it be known that his staff would give every help to any requests for radioisotopes for medical or medical research work. I went to see Gleep and discuss ideas with the staff. The reactor was in the middle of what had been an aircraft hanger and was encased in an immense wall and roof of concrete. There was a ladder, and we climbed up and walked around on the top to find several people conducting experiments. Some had pieces of string with which they lowered things down into the core, and then pulled them up again.
In the late 1940's, the Government decided that the top brass of the three Services needed to know something about the scientific background of the Atomic Bomb because it was going to be made in this country. I was told that Harwell ran a one-week course and that on the Friday afternoon there was an "any questions" session. The Admiral realised that he was the senior officer present, so moved a vote of thanks for the further horizons widened, the deeper vistas explored, and so on. However, he added that he would be glad if someone would explain in simple terms for him just what was the difference between a röntgen, a rad and a gonad.
The possibility of having radioactive tracers available prompted many in medical research to think what uses they could make of them. At the time, I was the only person at UCH who knew anything at all about radioactivity and Geiger counters - not much, but I learned quickly. Anyone in the Hospital or Medical School who considered using radioisotopes therefore came to me for help, and I collaborated in a number of research projects.
The first, and perhaps the most interesting in a general sense, came from a woman doctor on the Obstetric Unit. She had observed that a number of women in late pregnancy would develop "white leg" syndrome which is now called deep vein thrombosis in the calf. She thought it might result from the head of the baby being so firmly pressed into the pelvis that it partially obstructed the blood in the femoral vein as it entered the pelvis from the upper leg. This could cause the blood to run more slowly than usual and therefore for the corpuscles to be able more easily to attach themselves to the vein walls and start a blood clot. Could we use these new isotopes to measure the speed of the venous blood in the leg? We devised a method of injecting a little Na24 as saline into a vein in the foot, and checking its arrival at the groin with a shielded Geiger counter. We tested the method out on 100 normals - well they were medical students and nurses, but we called them normal for this purpose. We then tested some pregnant ladies and found that a small group of them had a blood flow about 1/3 of normal, which reverted to normal immediately after the delivery of the baby. We then tested people who in those days were subjected to complete bed rest - heart patients, and post-operative patients generally - and found that slowing of the blood flow was closely related to the incidence of thrombosis. If therefore when you have your next operation you are bullied out of bed the following day, you can blame this on the work of Osborn and Wright from 1950. You can also blame the accountants who have more recently had their say on this.
Another project involved injecting micro-spheres of radioactive glass into a patient and measuring the rate of clearance from the blood stream. Usually, as expected, the count rate between the thighs would fall in a more or less exponential way. Sometimes, however, there was a sudden rise in the count rate, followed by a fall exactly the same as we would have expected had there been no rise. After a few minutes, there would be a sudden drop down to the level we would have expected in the absence of any sudden rise. We tried to identify a cause for this, as it appeared to be totally unrelated to the count rate from the patient's thighs. Eventually we realised that the laboratory used was on the same level as the Radiotherapy Department. If one particular treatment room was being used with the beam pointing towards the window, any X-radiation emerging could be scattered from a wall a few feet outside the window. This again could be scattered by another wall some 40 feet away and just outside our laboratory, a little radiation entering our window. It seemed quite incredible that this might be the cause until we checked that the times for our sudden changes of count rate coincided exactly with the times of operation of that X-ray tube.
Life was not all radiation. For example. I normally had lunch with some of the medical staff, and one day I heard about a patient that had come in with a badly smashed jaw. The surgeon had used the good old RAF technique of manipulating all the pieces into place, putting a stainless steel pin in each and fixing them all to a stainless steel frame to which was also fixed the silver straps to keep the upper and lower teeth correctly aligned. Unfortunately, ulcers had developed round each of the stainless steel pins, and these just would not heal. I offered the help of Physics, and found a potential of about 0.5 volt between the silver straps and the stainless steel pins resulting in a current short-circuiting through the patient. I went back to my lathe and made up some insulating washers which I inserted between the silver straps and the stainless steel bar. Those ulcers disappeared overnight.
One morning I had a call from the Department of Physical Medicine. They had just bought a now type of amplifier and it was not working properly. It was about the size of a radiogram, and had two electrodes which were intended to be inserted into a patient's muscle. The instrument would then show on the oscilloscope the waveforms of the electrical signals; their average magnitude would be indicated on a meter, and a loud speaker would reproduce their sound. Unfortunately, the first patient was rather worried because all the loud speaker could emit was the radio "Morning Service". I got there during the afternoon in time for "Choral evensong" to find that they had just not earthed the patient properly, and he was acting as an aerial.
In 1952 the world's first thermonuclear bomb was tested, and the radioactive fallout shot up into the stratosphere to fall out all over the world in subsequent months. The Medical Research Council realised that this fallout might just cause genetic effects in the population of the UK as a whole, and that this should be investigated. They did the proper British thing, and set up a committee to look into it, who quickly realised that they had no idea how big or how small such an effect might be. They therefore decided that, at the same time and for comparison, they would try to find out what order of genetic hazard to the population there might be in the UK as a result of other sources of radiation. Among these were the radiation from cosmic rays, especially in aircraft crew, and the medical uses of X-rays and radioactivity. The work I had done on the radiation doses to diagnostic X-ray patients caused them to ask me to join them and make an estimate of the average amount of radiation likely to be received by the gonads of the average UK citizen from this source. There was little to go on, but I made an estimate which turned out to be of the same order of magnitude as that due to natural radioactivity. When the MRC report was published, it was debated in the House of Commons! It was the only time I have heard politicians trying to debate a scientific matter. I learned little except that a young lady Labour MP with very red hair made herself a nuisance by persistently asking the Minister questions about nuclear bombs, which were irrelevant to the debate. Here name was Barbara Castle. In replying to the debate, the Minister announced that he was setting up a Committee under the chairmanship of Lord Adrian, Vice-chancellor of Cambridge University, to look into radiological hazards to patients. This turned out to be a big operation, most of the scientific work being run by Prof. Spiers of Leeds, a member of the Committee, Roy Ellis, then of the Middlesex Hospital, and myself.
I had for some years realised that I really needed to have a PhD, and it was clear that this would provide the necessary material. I arranged for the Ministry of Health to write to UCH asking them to release me sufficiently from my routine duties to carry out this work for the Committee, which was accepted with great reluctance by UCH. The work has been fully reported in the literature. As far as I was concerned, it took 4½ years out of my life. Anyway I duly received my London PhD in 1961, just 20 years after my BSc.
In 1962 I was invited to King's College Hospital as Director of the Medical Physics Department with the status of Consultant. I was now in charge of my own Department, and no longer part of a Radiotherapy Department. Soon after I arrived at King's I was having a discussion in the office of the House Governor (i.e., chief executive) when there was a telephone call for me from the World Health Organisation in Geneva. I was asked to deputise for Prof. Mayneord in a lecture tour on radiation protection in Diagnostic Radiology in the Middle East, together with Prof. Dick Chamberlain of Philadelphia. Mayneord was ill, and so ill that he had suggested my name. The House Governor had previously served at the Royal Cancer Hospital (Free) and knew and respected Mayneord, so the strings were pulled and I found myself able to visit five Middle East countries in three weeks.
It was pretty hard work, involving visits to hospitals as well as giving lectures. Within weeks of this, I was asked to deputise for Mayneord again, this time on the design and production of a General Purpose X-ray Unit for developing countries. WHO had had one of their staff physicians invalided home with what turned out to be gross overexposure to X-rays because the machine he had been using was almost totally deficient in radiation protection. Mayneord had been on the design team for the new machine, and the draft specification had been sent to a number of X-ray manufacturers with the comment that when they had something like this, WHO would send a team to inspect it. They all replied predictably to say that they had nothing exactly like that available at the moment; they were sure that the WHO team would like to look at their new model AB7YZ, which was very similar.
Over the next year, we visited one firm in London, one in Holland and two in Germany. None of their offers could be accepted without modification, and we had to visit one four times before their machine could be accepted. WHO placed orders for one of each, to be installed in four similar village hospitals in Kenya. After they had been there for six months we were asked to inspect them to check that all the parts had arrived and been correctly installed, that none had already rusted through, and so on. In one village I protested that the installation had not been carried out as I had recommended. As a result if it were necessary to direct the beam across the table, it would go on either straight at the radiographer at the control panel, or out of the door to irradiate the queue of patients patiently waiting their turn. They protested that my proposal was impossible since one of the cables was too short. The specification was immediately altered so that that cable had a break for an extension cable to be inserted on site if necessary.
I was a part-time consultant to WHO for 15 years and came across many interesting, and not a few horrifying, sights during visits to some 15 countries. I was sent to Indonesia to set up a film badge service for their hospitals - their nuclear energy set-up had one, but wouldn't share it. I visited the country's newest University Hospital - it had achieved this status only a couple of months before. After the usual coffee in the Hospital Director's office, I asked if I could meet the radiologist in charge of the X-ray Department. No, we don't have a radiologist. What about the doctor in charge, then? No doctor. Then who is in charge of the Department? Oh, the radiographer. Can I meet him? No, he is away on a course this week. Who is running the Department today? Oh, the darkroom technician. Could I meet him? Of course. He asked us what to do with the knob labelled kV. He had it set at 60 for everything. But his greatest worry was that the surgeons sent him patients who had just had fractures set, with the request that he, the darkroom technician, should say whether the result was satisfactory. And this was in a University Hospital!
Soon after I went to King's, I was involved in a project that might be of interest. After a scientific meeting I was approached by a health physicist from Aldermaston, then concerned with nuclear weapons. He had a detector arranged to be particularly sensitive to the 2 MeV radiation from sodium24. Some of the natural sodium in a person exposed to neutron irradiation would be transformed to sodium24, and a rough measurement of this could give a quick indication of the magnitude of the neutron exposure. However, he needed to calibrate this in terms of the amount of sodium24 in the body, and he didn't want to arrange a nuclear explosion for the purpose. Did we ever inject sodium24 into patients for medical purposes, and if so could he try out his counter on some of them? It so happened that John Anderson, our Professor of Medicine, was interested in body sodium, and was carrying out just the kind of sodium24 injections required. The counter was tried, and a calibration figure obtained. It struck me that there was no satisfactory method of determining the amount of sodium actually in the body of a patient. Input and output could quite easily be determined, but not body content. It occurred to me that we could turn this idea round. Instead of assuming body sodium content, and calculating the neutron exposure from the sodium24 produced, we could administer a whole-body neutron dose of small but known magnitude, measure the sodium24 produced, and calculate the body content of sodium. We approached Harwell, and got permission to carry out such experiments during the night when the necessary neutron generator would be available. A trial run in which both John Anderson and I were irradiated showed that the method was feasible, and a good deal of work on the physics of this gave my colleague Keith Battye his Ph.D. We then applied for research funds for both a neutron generator and a whole-body monitor, but the cost was going to be enormous. So the funds went instead to two institutions; one already had a neutron generator, and only wanted a whole body monitor, while the other had a whole body monitor and only needed a neutron generator. Ah, well; that's life!
I could go on about recent developments in Medical Physics, things like CT scanning, Magnetic Resonance Imaging, the many uses of electronics, ultrasound, medical engineering, and so on and so forth. Most people currently in Medical Physics are more familiar with these and other recent developments than I am, who retired 25 years ago. I have therefore concentrated on what the profession was like in the first half of the 60 years in my brief. There are many more stories I could tell, but I will only bore you with one more.
In about 1948 therapeutic quantities of I131 became available, and a patient with a very large cancer of the thyroid came to UCH from abroad for treatment. The medical staff asked me to get hold of as much I131 as I could very urgently for her treatment. I managed to get 80 mCi,(i.e., 30 GBq) and it was arranged to administer this the same afternoon. Just before leaving that evening I went to the ward to see that all was well, to find that she had had a relapse, was incontinent and was likely to die during that night. I explained to Sister that when she did die certain precautions would need to be taken. She still had most of the radio-iodine in her body, but some would be in her urine and also in the bed. I offered to come in at any hour as required, but that in any case the nursing staff could close her eyes, so long as they left the body in the Ward (against all normal requirements). Sister said that if I briefed the Night Sister sufficiently the rest could wait till morning.
At 9 the next morning the patient was still in her bed, having died about 3 o'clock. I got four nurses gowned and gloved to contain contamination. They lifted the body up while I put the sheet and the water-proof under-sheet into a dustbin and replaced them with a plastic sheet. I supervised what are known as "last offices" and then went and had a well-earned cup of coffee. I was then approached by the Ward Sister who said that the relatives had asked for cremation, so that they could take the ashes (and much of the radioactivity!) back home with them. I said that this would be too dangerous, and insisted on an ordinary burial. It then turned out that she was a Jewess. Had she been a strict Jewess, I was told, all the last offices would have had to be performed by a Rabbi, and on his own. However, Rabbis have no more training in radioactive contamination than do Medical Physicists in theology. This suggested to me that we might have difficulties in similar circumstances with patients of other faiths.
Together with the Ward Sister, I conducted a survey. For example, for a Muslim any surgical intervention after death would have to be approved in advance by an Imam. For a Hindu, cremation would be imperative, and the same day if at all possible. For a Jehovah's Witness, a Watcher would have sat by the bedside until death, radiation hazards or not. And so on. So we wrote a joint letter to the Hospital Administration making a suggestion in case this situation ever arose again. We suggested that I should be instructed to ensure that, as far as possible, we avoided contravening any religious tenets of the distraught relatives. I should apply normal radiation protection procedures as far as I could, but that if this would cause distress to the relatives, I was authorised to take whatever minimum steps were necessary to avoid this. But it never happened again in my time. When the Ionising Radiation Regulations were being drafted I tried to get some wording inserted to the same effect, but was told that this would contravene the wording of the European Directive. I said that it was obvious that the European Directive was in error, but this cut no ice. Nevertheless, I was given a verbal assurance that in such circumstances a hospital would never be prosecuted for taking appropriate action. There is still nothing to that effect in writing.
I have just realised that this is the first time I have mentioned the Ionising Radiation Regulations. They began when the European Community set up a scientific Committee to consider the need for such regulations in member states, and the general form they should take. In due course, each Member State received a Directive, saying that all Statestogether with a radiologist from Lancashire who could not attend very often, had the responsibility of looking after the interests of the Health Service.
Now the philosophy of radiation protection of a worker is quite different from that of a patient, and a good many modifications to the initial proposals had to be made, especially concerning volunteers in research projects. Another was concerned with the movement of radioactive sources. The draft said, in effect, that if radioactive material had to be moved between one building and another, it MUST be in a secure, leak-proof, container. I said we could not accept that in hospitals. I pointed out that we very often put small quantities of radioactivity into patients for test purposes, and then sent them home. As at present, we would be only prepared to send home in a sealed, leak-proof container those patients who would never, ever, be able to return for further treatment. This regulation now has a sentence at the end which says "unless the radioactive material is in or on the body of a person for medical purposes. There were many other matters that had to be raised. I consulted my medical physics colleagues about the draft regulations several times. I often said that when all was said and done, no-one would notice the hundreds of small matters that had been put right, and attention would be focussed on the two or three that we tried to alter, but failed. The need to be able in appropriate circumstances to deal with a patient with consideration and sympathy, and not just mechanically according to rule, was one of these.
This has been a personal reminiscence of the earlier days of Medical Physics which I would not wish to inflict it on any physicist today, although life was in some ways simpler then. I came into our profession primarily to contribute what skills I had for the benefit of sick patients. Yes, we are physicists, but we are also health workers, and I have been greatly gratified to see the constantly widening field of Medical Physics that today is available for the benefit of sick patients.
Reference
1. Chalmers T. A. Brit J Radiol. Vol vii 1934 p 756.
Glossary of abbreviations